Back from the Edge…
Non-Alcoholic Steato-Hepatitis (NASH), GERD, Shortness of Breath, Chronic Fatigue
This is the clinical history and results of a patient enrolled in a personalized nutritional program with our sister company, Veritas Health Analytics.
History:
This patient is a 70 year old female with chief complaints of:
Chronic fatigue
Reflux and heartburn (GERD)
- Coronary artery stents
- High cholesterol
- Hypertension
- Overweight
- Shortness of breath
- Stress incontinence
- Urinary frequency
Medications:
- Aspirin
- Metoprolol
- Cozaar
- Metamucil
- Lipitor
- Tylenol (periodically)
- Prilosec
- Tums
This patient was finally taken off Lipitor when her liver enzymes had been continually trending upwards over a period of three years. Unfortunately for this patient, when the Lipitor was withdrawn, damage had already been done to her liver in the form of cirrhosis resulting from non-alcoholic Steatohepatitis (NASH). All medications put an increased toxic burden on the liver, and as such, are contributory in the genesis of NASH.
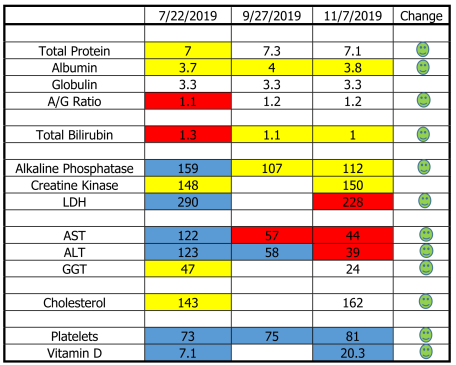
Baseline Testing: July, 2019
Our baseline blood testing was performed to elucidate the extent of liver inflammation and function and establish the mechanisms by which the body was adapting to the liver dysfunction. Hair analysis was also performed to determine the toxic load on this patient’s body, how able she was to eliminate toxins and quantify her essential mineral reserves.
Her liver’s ability to maintain protein balance in the blood was impaired.
Albumin yellow (warning) low
Albumin/Globulin Ratio red (emergency) low
The history provided evidence of inefficient protein digestion based on reflux and Prilosec use.
Total protein yellow low
She was breaking down muscle tissue to meet protein demands.
Creatine Kinase yellow high
LDH blue (critical) high
The liver’s ability to clear the blood of bilirubin had been decreased.
Total bilirubin red high
Liver enzymes were critically high indicating inflammation and liver cell death.
Alkaline Phosphatase blue high
AST blue high
ALT blue high
GGT yellow high
Cholesterol was yellow low. (A sign of a sick liver)
Platelets were dangerously blue low.
Yellow = Warning Red = High Risk Blue = Critical
Her Nutrition Program:
The main dietary changes here were to increase protein intake, decrease carbohydrate load and increase good fats. An intensive supplementation regimen was embarked upon based upon our findings of her complete analysis which included antioxidants, probiotics, a chelating agent, support for detoxification reactions, liver defatting supplements, omega 3 oils, electrolytes, trace minerals, digestive enzymes and vitamin D.
Follow Up Testing:
Due to the seriousness of this patient’s situation, follow up testing was done at shorter intervals to monitor the effect of our program. All indicators except for the creatine kinase (which was essentially unchanged) have improved. Liver enzymes have improved dramatically.
Serum proteins are beginning to rebound
Liver is clearing bilirubin better
Alkaline Phosphatase has been reduced by 30%
LDH has come down 21%
AST has been reduced by 64%
ALT is down 68%
GGT is 49% less
Cholesterol is up (and yes, that is good) 13%
Platelets are slowly improving
Vitamin D has improved markedly, (up 186%) but there is still a ways to go
Results of Her Program:
This patient was in a very bad situation with her liver. The liver controls and carries out so many biochemical processes. The truth is that you can’t live without a liver. The good news is that the liver is fairly resilient and can recover somewhat as long as stressors to it are reduced and it is supported nutritionally.
Aspirin, Tylenol, Lipitor, Prilosec and Tums are no longer being used. We will continue to monitor blood pressure, pulse rate and blood oxygenation in the desire to reduce the heart meds in the future.
In this case, liver failure and the need for a transplant has been averted. We continue to work together and just received the results of more testing indicating an even further reduction in liver enzymes.
This patient has done a fine job in sticking to her program and is now reaping the results of her efforts. I can imagine what would have become of her if the destruction of her liver was allowed to continue. We will continue to support, detoxify, retest and adjust our protocols, but we are indeed moving the ball in the right direction